Pediatric brain cancer prediction is a rapidly evolving field that harnesses the power of AI in pediatric oncology to better understand the complexities of brain tumors in children. Recent advancements have led to the development of innovative tools that accurately assess brain cancer relapse risk, particularly in cases involving gliomas. Traditional methods of monitoring these cases often fall short, yet breakthroughs in MRI for brain tumors and emerging techniques like temporal learning in medicine provide fresh hope. As researchers explore glioma treatment advances, the application of AI may allow for earlier identification of patients at high risk, transforming their follow-up care into a more manageable process. Ultimately, the goal of these innovations is to improve outcomes and reduce the burden on both young patients and their families.
The exploration of pediatric brain tumor forecasting represents a significant leap in medical technology. By utilizing artificial intelligence, medical professionals can enhance the prediction of recurrence in childhood brain cancers, specifically focusing on gliomas. This development underscores the importance of advanced imaging techniques, such as magnetic resonance imaging, which are crucial in assessing tumor dynamics. Furthermore, novel approaches like chronological learning bring a fresh perspective on how we understand and anticipate the progression of these diseases. This shift towards automated analysis not only promises better management strategies but also alleviates the psychological strain on children undergoing frequent clinical evaluations.
Understanding Pediatric Brain Cancer Relapse Risks
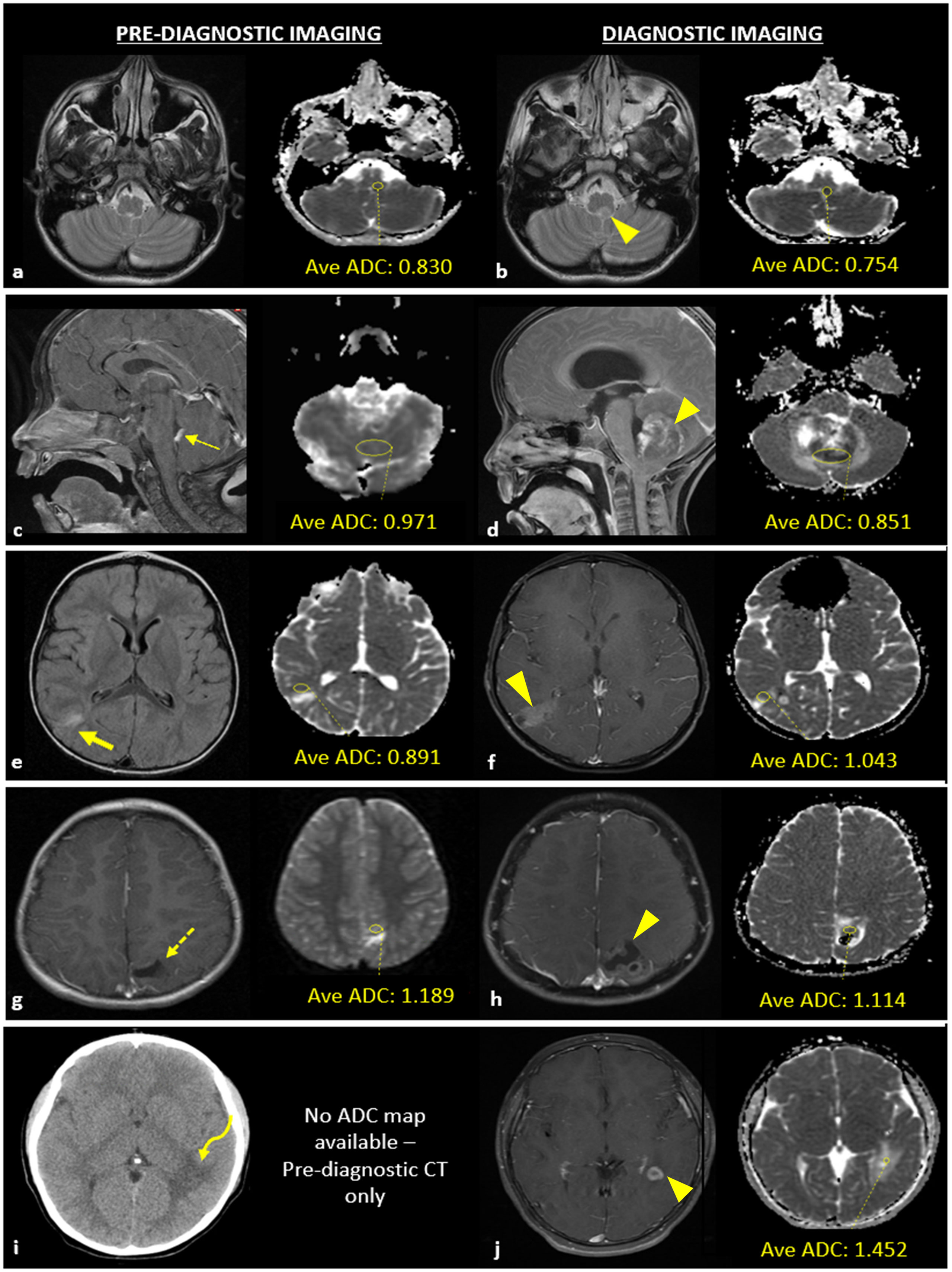
Pediatric brain cancer, specifically gliomas, presents a complex challenge in the medical community, primarily due to the risk of recurrence after initial treatment. Traditionally, pediatric oncologists have relied on standard follow-up protocols, including regular MRI scans, to monitor patients post-surgery. However, these methods can often yield uncertain results, making it difficult to foresee which patients might be at an increased risk of relapse. Recent advancements in artificial intelligence (AI) are shifting the landscape of pediatric oncology by providing the ability to analyze multiple scans over time, thereby offering a more nuanced prediction of brain cancer relapse risk. By leveraging AI tools, healthcare professionals can enhance their understanding and approach to monitoring these vulnerable patients more effectively.
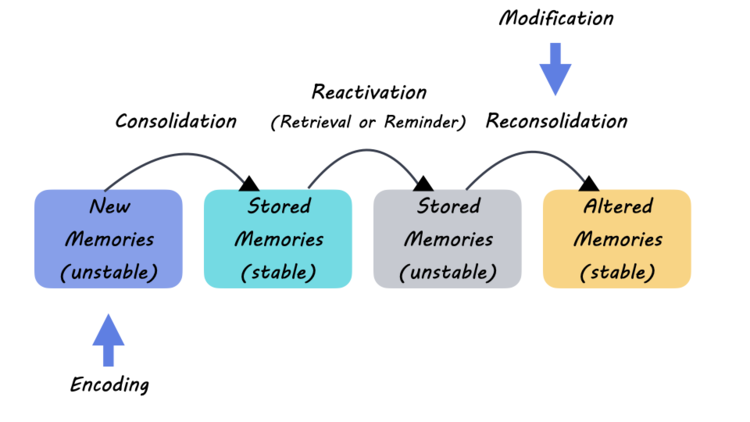
This innovative AI-based prediction model utilizes temporal learning—an approach that synthesizes data from several MRIs over months—allowing for a more comprehensive analysis of changes in the brain over time. Unlike conventional single-scan evaluations, this method enhances the accuracy of detecting emerging tumor activity and provides essential insights into the potential for disease recurrence. As Benjamin Kann mentions, this shift towards better predictive tools not only alleviates the anxiety associated with frequent imaging but also paves the way for personalized treatment strategies tailored to individual patients’ risk profiles.
The ability to predict which pediatric glioma patients are most at risk of recurrence holds profound implications for treatment protocols. By identifying those at high risk early, clinicians can initiate targeted therapies sooner, potentially improving outcomes significantly. AI in pediatric oncology marks a paradigm shift in how cancer management is approached, allowing healthcare providers to forego unnecessary stress imposed by frequent follow-up scans for patients at lower risk. The overarching goal of these predictive tools is not just to enhance accuracy but to foster a holistic approach in managing the psychological and physical toll that ongoing cancer treatments can exert on children and their families.
Innovations in Glioma Treatment Advances
Recent studies underscore the rapid pace of advancements in glioma treatment methodologies, particularly as they intertwine with artificial intelligence. The integration of AI in analyzing patient data, such as MRI scans, offers a fresh lens through which to view treatment efficacy. Trials are currently underway where AI tools assist in customizing glioma treatment based on predicted relapse risks decoded from temporal learning approaches. This represents not only a leap forward in technology but a concerted effort to improve the quality of life for pediatric patients afflicted with brain tumors.
Moreover, ongoing research efforts in glioma treatment focus on exploring adjuvant therapies for high-risk patients as indicated by their AI-derived risk profiles. The hope is to develop treatment algorithms rooted in AI analysis that can dictate when to intensify or modify treatment regimens based on reliable predictions of recurrence risk. As breakthrough insights evolve from these AI applications, they will shape future glioma treatment protocols, melding advanced imaging technologies with cutting-edge AI capabilities to elevate care standards in pediatric oncology.
The Role of Temporal Learning in Pediatric Oncology
Temporal learning is emerging as a transformative factor in pediatric oncology research, particularly for conditions like gliomas that require vigilant monitoring. By employing algorithms that analyze a succession of MRIs rather than stand-alone scans, researchers can detect trends and subtle changes that signify potential tumor recurrence. This progressive approach reflects a broader trend within medicine that emphasizes predictive analytics—empowering healthcare professionals to make preemptive and informed decisions based on extensive datasets.
Implementing temporal learning in clinical practice could revolutionize traditional monitoring practices for pediatric cancer patients. As these AI models grow increasingly sophisticated, they will enable earlier intervention strategies, ultimately leading to better health outcomes. By harnessing vast datasets from prior patient imaging, the medical field can foster a proactive rather than reactive methodology—ensuring children with brain tumors receive optimal care tailored specifically to their unique circumstances.
Enhanced MRI Techniques for Brain Tumor Monitoring
MRI technology continues to evolve, presenting exciting prospects for improving brain tumor monitoring, especially in pediatric patients. Recent developments have led to enhanced imaging techniques that, when combined with AI analysis, result in superior visualization of tumor characteristics and behavior over time. This not only aids in the identification of glioma recurrence but also provides vital information regarding tumor dynamics that can guide treatment strategies. Furthermore, leveraging MRI data synergistically with AI can lead to innovative diagnostic tools that streamline the monitoring process for young patients.
As pediatric brain cancer cases rise, the optimization of MRI technologies becomes paramount in delivering high-quality care. The incorporation of advanced imaging modalities that work hand-in-hand with AI tools offers the potential for earlier detection of changes associate with tumor recurrence. These advances promise improved surveillance protocols that minimize patient burden and increase clinical efficiency, ultimately leading to better outcomes for children diagnosed with gliomas.
AI-Driven Precision Medicine in Pediatric Oncology
The advent of AI-driven precision medicine marks a pivotal juncture in the management of pediatric brain cancers. By utilizing AI algorithms to analyze extensive datasets from multiple brain scans, clinicians are able to craft individualized treatment plans that take into account each patient’s unique tumor characteristics and recurrence risk. This precision approach aligns treatment modalities directly with patient needs, enhancing the efficacy of interventions while reducing potential side effects associated with unnecessary therapies.
Precision medicine in pediatric oncology represents a holistic shift towards incorporating genetic, biological, and imaging data to inform treatment decisions. As AI tools become more prevalent within oncology practices, the integration of predictive algorithms can radically change the landscape of treatment for pediatric gliomas. This ongoing evolution emphasizes the critical importance of personalized care and proactive management, ensuring that every child receives the most supportive and effective treatment based on their specific circumstances.
Predictive Analytics: Transforming Patient Care in Oncology
Predictive analytics is fundamentally transforming the approach to patient care in oncology, particularly in the realm of pediatric brain cancers. With the ability to extract valuable insights from extensive imaging data, predictive analytics enables healthcare professionals to forecast treatment outcomes with greater accuracy. This proactive stance in patient management allows for timely interventions that can significantly improve prognoses, particularly for those at risk of glioma recurrence, as highlighted by recent studies employing AI technologies.
As healthcare systems embrace predictive analytics, the goal is to cultivate a data-driven culture that prioritizes evidence-based decision-making. This initiative not only optimizes the quality of care but also streamlines the patient experience, reducing the burden of frequent imaging and evaluations. Such advancements represent a promising future where patient care is not merely reactive but anticipative, ultimately leading to enhanced survival rates and better overall quality of life for children battling brain tumors.
Challenges in Effective Brain Cancer Monitoring
Despite the advancements in AI and MRI technologies, several challenges remain in the effective monitoring of pediatric brain cancer patients. Establishing standardized protocols that integrate these new predictive tools into routine clinical practice presents its own set of hurdles. Training clinicians to rely on AI-driven insights while navigating the traditional methods they have employed for years is an ongoing process. This transition is essential to realize the full potential of AI in enhancing the accuracy of monitoring brain cancer recurrence.
Additionally, ethical considerations regarding the extent of AI deployment in patient monitoring must be addressed. As AI technologies gain prominence, ensuring that these tools are utilized responsibly and transparently is paramount. Researchers and practitioners must collaborate to establish guidelines that govern the implementation of AI tools in pediatric oncology, promoting patient safety while optimizing cancer treatment pathways. Addressing these challenges head-on will ensure that the shift toward automated predictive analytics is safe and beneficial for young patients.
The Future of Pediatric Oncology with AI Insights
The future of pediatric oncology, particularly regarding brain cancer, appears promising with the ongoing integration of AI insights. As researchers continue to refine AI algorithms, the potential for breakthrough discoveries in monitoring, diagnosing, and treating pediatric gliomas expands exponentially. Aiming for precision in predicting patient outcomes, these insights not only help in tailoring treatments but also foster a deeper understanding of the tumor biology that governs glioma behavior, thus paving the way for innovative therapies.
Moreover, as community-wide clinical trials begin to incorporate AI-powered tools, the opportunities for collaboration between institutions will likely grow. This will usher in a new era of shared knowledge and data that informs best practices in treating pediatric brain tumors. By facilitating an informed and engaged network of healthcare providers, we will move toward a robust framework of care that ensures that every child has access to cutting-edge treatment options and support as they navigate their cancer journey.
Educational Initiatives Supporting Pediatric Brain Cancer Awareness
Raising awareness about pediatric brain cancer and fostering a culture of education surrounding the condition is crucial for early detection and intervention. Educational initiatives targeting healthcare providers, families, and communities play an integral role in demystifying the complexities associated with gliomas and their treatment options. Understanding the signs and symptoms of brain tumors can empower parents to seek timely medical advice, potentially improving outcomes for affected children.
Incorporating AI insights into these educational efforts further enhances the endeavor by providing succinct, evidence-based information regarding symptomatology, monitoring strategies, and treatment advances. By distributing knowledge through seminars, workshops, and community outreach programs, healthcare systems can bridge the knowledge gap, ensuring that families are equipped with the necessary tools to advocate for their children’s health. Heightened awareness and understanding will ultimately lead to more vigilant monitoring practices and a stronger network of support for pediatric cancer patients.
Frequently Asked Questions
How does AI improve pediatric brain cancer prediction compared to traditional methods?
AI enhances pediatric brain cancer prediction by analyzing multiple brain scans over time, which allows for a more accurate assessment of relapse risk in children diagnosed with gliomas. Traditional methods often rely on single scans, which do not capture subtle changes indicative of recurrence. The use of temporal learning in AI models has demonstrated a prediction accuracy of 75-89%, significantly outperforming the approximately 50% accuracy of single-image predictions.
What role does MRI play in pediatric brain cancer prediction?
Magnetic Resonance Imaging (MRI) is crucial for pediatric brain cancer prediction as it provides detailed images of the brain that help detect tumors and monitor changes post-treatment. In the context of glioma treatment, MRI scans are analyzed using advanced AI tools to assess the likelihood of cancer relapse, thus aiding in better treatment planning and follow-up strategies.
What is temporal learning and how is it used in pediatric oncology?
Temporal learning is a novel AI technique that trains models to analyze sequences of brain scans taken over time, rather than relying on isolated images. In pediatric oncology, this approach allows researchers to identify subtle changes in brain tumors, such as gliomas, that may predict the risk of recurrence. This continuous assessment improves the accuracy of risk predictions, leading to more tailored treatment strategies.
How are advances in glioma treatment related to pediatric brain cancer prediction?
Advances in glioma treatment are directly linked to improvements in pediatric brain cancer prediction through the use of AI and temporal learning. By accurately predicting relapse risks, clinicians can better personalize treatment plans, potentially reducing the need for certain interventions while ensuring high-risk patients receive timely and appropriate care.
What implications does AI in pediatric oncology have for family stress levels?
The use of AI in pediatric oncology, especially for predicting brain cancer relapse, has the potential to lessen family stress levels. Frequent follow-ups and MRIs can be burdensome; however, enhanced prediction models may reduce unnecessary imaging for low-risk patients, making the process less stressful for families while optimizing care for those at higher risk of recurrence.
What are the potential future applications of AI in pediatric brain cancer management?
Future applications of AI in pediatric brain cancer management include improved prediction of cancer recurrence using temporal learning models, tailored treatment plans based on risk assessments, and possibly minimizing hospital visits through targeted imaging based on AI-informed predictions. Clinical trials are anticipated to explore these possibilities and refine how AI can enhance outcomes in pediatric oncology.
| Key Points | Details |
|---|---|
| AI Tool for Predicting Relapse | An AI tool demonstrates enhanced accuracy in predicting the risk of pediatric brain cancer relapse compared to traditional methods. |
| Focus on Pediatric Gliomas | The study particularly targets gliomas, a type of brain tumor in children that can be treated successfully but carries risks of return. |
| Temporal Learning Technique | Researchers utilized a new AI approach called temporal learning, analyzing multiple MR scans over time for better predictions. |
| Accuracy of Predictions | The AI tool achieved 75-89% accuracy in predicting relapse one year after treatment, outperforming traditional single-scan methods (50% accuracy). |
| Future Clinical Applications | The researchers aim to validate these findings and potentially initiate clinical trials to improve patient care based on AI predictions. |
Summary
Pediatric brain cancer prediction has advanced significantly with new AI technologies developed to accurately forecast the risk of relapse in young patients. This innovative approach, particularly for pediatric gliomas, highlights a pivotal shift from traditional single-scan assessments to a more sophisticated analysis of multiple scans over time. By employing temporal learning techniques, researchers have achieved remarkable improvements in accuracy, which could transform follow-up care and treatment strategies for children at risk of recurrence.