Pediatric cancer recurrence poses a significant challenge, especially in young patients diagnosed with brain tumors like gliomas. Recent advancements in AI in pediatric oncology have revolutionized how health professionals assess the risk of relapse. By utilizing innovative techniques such as temporal learning, researchers have improved the predictability of cancer relapse, leading to more informed treatment strategies. This not only alleviates the psychological burden of frequent imaging on families but also enhances the overall quality of care. With a focused approach to brain tumor risk assessment, this new methodology promises to transform outcomes for children facing the threat of pediatric cancer recurrence.
The re-emergence of cancer in children, particularly following initial treatment, remains an urgent concern for healthcare providers and families alike. Alternative methodologies for predicting cancer relapse are emerging, leveraging advanced technologies and data analysis, including exciting techniques like temporal learning in medical imaging. These innovations offer hope for improved management of conditions such as pediatric gliomas—brain tumors that often require delicate treatment strategies to minimize the risk of return. As experts delve deeper into brain tumor risk evaluation, the emphasis on better prediction tools is vital to enhancing pediatric cancer care and recovery outcomes. By harnessing AI-driven insights, the future holds promise for significantly reducing the stress associated with follow-up treatments.
Understanding Pediatric Cancer Recurrence and Its Challenges
Pediatric cancer recurrence is a significant concern for healthcare providers and families alike. After initial treatments, such as surgery and chemotherapy, some children may face the terrifying possibility of their cancer returning. This situation, especially prevalent in cases like pediatric gliomas, underscores the need for precise risk assessment methods to guide treatment decisions and follow-up care. Traditional methods of monitoring often fall short, relying on periodic imaging that may not effectively identify which patients are at the greatest risk of relapse.
The emotional burden of repeated imaging procedures can weigh heavily on children and their families. Increased anxiety and stress accompany the uncertainty of outcomes, as families are often left waiting and worrying about the return of cancer. New advancements using AI in pediatric oncology are being explored to alleviate these burdens by providing more accurate predictions of relapse risk, ultimately leading to tailored, less invasive follow-up strategies.
The Role of AI in Predicting Cancer Relapse
Artificial intelligence has revolutionized many fields, and medicine is no exception. In pediatric oncology, AI tools are emerging as powerful allies in predicting cancer relapse. Research from Mass General Brigham demonstrated that AI-driven analysis of multiple magnetic resonance imaging (MRI) scans can significantly enhance the accuracy of predicting the likelihood of recurrence in pediatric glioma patients. By leveraging vast datasets and advanced algorithms, these AI systems analyze subtle changes over time that might be easily missed by the human eye.
The incorporation of temporal learning into AI models allows for a more comprehensive understanding of a patient’s condition. Instead of relying solely on isolated scans, these AI systems interpret trends across various imaging sessions, leading to more informed predictions. As a result, clinicians can better stratify patients based on their individual risk profiles, allowing for more focused interventions and potentially sparing low-risk patients from the anxiety of frequent imaging.
Advancements in Glioma Treatment and Monitoring
Glioma, a type of brain tumor that is more common in children than adults, presents unique treatment challenges. Traditionally, treatment has involved surgery, followed by chemotherapy or radiation, but the risk of recurrence necessitates ongoing monitoring that can be both invasive and emotional for young patients. Recent innovations in AI and the use of temporal learning techniques have the potential to transform how clinicians approach glioma treatment and follow-up care, enabling personalized strategies based on individual response to therapy.
The promise of improved treatment protocols arises from these advanced predictive models. They not only identify patients who may benefit from more aggressive follow-up intervention, but also those whose treatment can be adjusted to minimize unnecessary exposure to imaging procedures. This shift toward individualized care reflects a broader trend in medicine where patient outcomes are prioritized through innovative technology and research-driven methodologies.
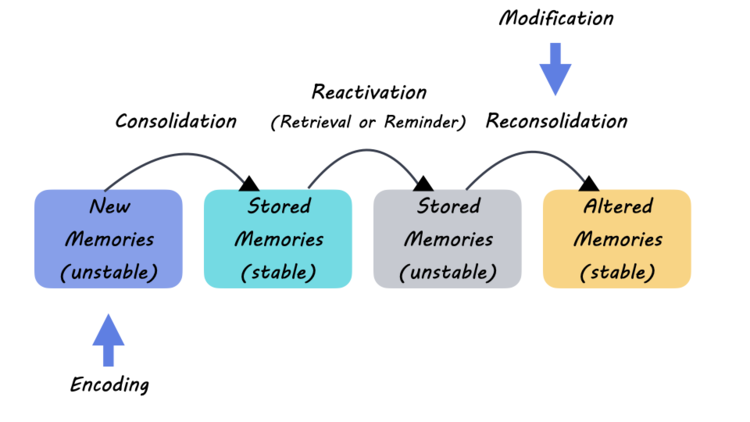
Utilizing Temporal Learning in Medicine
Temporal learning represents a groundbreaking approach in the medical field, particularly for patient monitoring post-treatment. Unlike traditional models that analyze single snapshots of patient data, temporal learning evaluates data trends over time. This methodology is particularly beneficial in pediatric oncology, where conditions can change rapidly, and early detection of relapse is vital for effective intervention. The ability to track subtle changes through sequential imaging can lead to timely and targeted treatment adjustments.
As this innovative learning process becomes more widespread, the implications for other areas of medicine are profound. By applying temporal learning principles, healthcare providers can gain deeper insights into disease progression and patient responses, ultimately enhancing the quality of care across numerous disciplines. This evolution towards a more dynamic understanding of patient health sets a new standard for how clinicians monitor and adjust treatment in real-time.
The Importance of Accurate Brain Tumor Risk Assessment
Accurate risk assessment for brain tumors, particularly in pediatric patients, is essential for determining the most effective treatment plans and follow-up strategies. With the complexity of brain tumors like gliomas, understanding the potential for recurrence can be the difference between successful treatment and more serious health complications. AI tools designed to predict pediatric cancer recurrence take risk assessment to the next level, using comprehensive data from imaging and patient history to refine the accuracy of these predictions.
These advanced risk assessment techniques harness machine learning to analyze vast amounts of medical data, providing insights that enhance decision-making in clinical settings. By integrating AI into routine assessments, healthcare professionals can confidently categorize patients into risk profiles and tailor their treatment plans accordingly. This level of precision not only optimizes resource allocation but also greatly benefits the psychological well-being of families by reducing unnecessary procedures.
The Future of Pediatric Oncology with AI Innovations
The future of pediatric oncology is poised for transformation, particularly with the integration of AI innovations. As evidenced by recent research, AI tools that analyze multiple imaging scans enable clinicians to predict pediatric cancer recurrence far more accurately than traditional methods. The prospect of reducing unnecessary imaging and focusing on high-risk patients demonstrates a significant leap towards personalized medicine in this field.
Healthcare providers are now equipped with the ability to utilize AI-driven insights to guide not only treatment but also the overall management of patient care. The emphasis on developing technologies that predict cancer relapse will likely result in better patient outcomes and less parental anxiety associated with treatment unpredictability. As these AI applications evolve, they hold the promise of revolutionizing pediatric oncology.
Reducing Imaging Frequency and Patient Burden
One of the key benefits of employing AI in pediatric oncology is the potential to reduce unnecessary imaging frequency for patients identified as low-risk for cancer recurrence. Traditionally, pediatric patients often endured regular MRI scans, leading to increased anxiety and logistical challenges for families. By utilizing predictive algorithms, healthcare teams can confidently decrease the number of follow-up scans required for patients less likely to experience relapse, thereby easing their burden.
The implications of this are profound not only for the patients but also for the healthcare system as a whole. By streamlining follow-up care through targeted imaging based on AI predictions, resources can be allocated more effectively, ensuring that high-risk patients receive the attention they need while lessening the emotional stress on families. This model redefines how pediatric cancer care can be delivered, supporting a more humane approach to treatment and recovery.
Enhancing Patient-Centric Care in Pediatric Oncology
The integration of AI in pediatric oncology represents a significant shift towards patient-centric care. With an emphasis on early detection and personalized treatment plans, this approach empowers families and healthcare providers to make better-informed decisions regarding care. By focusing on individual patient profiles, researchers and clinicians can leverage AI tools to enhance the overall experience and outcome for pediatric cancer patients.
Families are increasingly being engaged in the care process as predictive analytics provide them with clearer expectations regarding treatment paths and potential outcomes. This open dialogue fosters a stronger support system, which is critical in navigating the complexities of pediatric cancer. The alignment of AI innovations with patient-centric values reflects a growing understanding of the unique needs presented by pediatric populations.
Building Collaborative Networks for Pediatric Cancer Research
Collaborative networks among pediatric oncology researchers, hospitals, and technology developers play a crucial role in advancing the capabilities of AI applications. The integration of knowledge and technology from various institutions can drive meaningful improvements in predicting outcomes for pediatric cancer patients, including recurrences. As demonstrated in the Harvard study, partnerships among leading medical institutions allow for the pooling of resources, talent, and data, resulting in breakthroughs that can directly benefit patient care.
The commitment to fostering collaboration among different entities not only amplifies research output but also ensures that cutting-edge solutions are accessible to diverse patient populations. As more institutions participate in these networks, the potential for wider implementation of effective AI tools in clinical practice expands, ultimately leading to comprehensive improvements in the standard of care for pediatric cancer patients.
Frequently Asked Questions
What role does AI play in predicting pediatric cancer recurrence?
AI has emerged as a powerful tool in predicting pediatric cancer recurrence, particularly in brain tumors like gliomas. Through advanced techniques such as temporal learning, AI analyzes multiple brain scans over time, allowing for more accurate assessments of relapse risk compared to traditional methods that rely on single images.
How effective is temporal learning in the context of pediatric cancer recurrence prediction?
Temporal learning significantly enhances the prediction of pediatric cancer recurrence by synthesizing findings from multiple brain scans over time. In recent studies, this approach achieved accuracy rates between 75-89% for predicting glioma recurrence within a year after treatment, demonstrating its superiority over single-scan assessments which had only around 50% accuracy.
What implications does the AI study have for glioma treatment in pediatric oncology?
The AI study’s findings could transform glioma treatment in pediatric oncology by identifying patients at high risk of recurrence more accurately. If validated in clinical trials, this could lead to tailored follow-up protocols, reducing anxiety for low-risk patients and enabling targeted interventions for those at greater risk of relapse.
Why is it challenging to predict pediatric cancer recurrence in glioma patients?
Predicting pediatric cancer recurrence in glioma patients is challenging due to the variability in tumor biology and treatment response. Unlike many adult cancers, pediatric gliomas can often be managed with surgery alone, yet determining which patients are likely to relapse requires sophisticated imaging and monitoring, historically resulting in a lack of reliable predictive tools.
What are the potential benefits of using AI in brain tumor risk assessment for children?
Utilizing AI in brain tumor risk assessment for pediatric patients could lead to earlier, more accurate predictions of cancer recurrence. This advancement may facilitate personalized treatment plans, lessen the frequency of unnecessary imaging for low-risk patients, and improve overall outcomes by enabling timely interventions for high-risk individuals.
How can AI tools inform follow-up care for pediatric cancer patients?
AI tools can inform follow-up care for pediatric cancer patients by providing precise risk assessments based on historical imaging data. This capability allows healthcare providers to adjust surveillance strategies—offering less frequent imaging for low-risk cases and more intensive monitoring or treatment for those identified as high-risk for pediatric cancer recurrence.
What are the next steps after the AI study on pediatric cancer recurrence predictions?
Following the initial AI study on predicting pediatric cancer recurrence, the next steps involve further validation of the findings in diverse clinical settings. Researchers aim to initiate clinical trials to evaluate whether AI-driven risk predictions can effectively enhance patient management and treatment outcomes in pediatric oncology.
How can families prepare for the possibility of pediatric cancer recurrence?
Families can prepare for the possibility of pediatric cancer recurrence by staying informed about the patient’s condition, understanding the available monitoring tools including AI advancements in predicting relapse, and maintaining open communication with healthcare providers about follow-up plans and any changes in the child’s health.
What resources are available for parents dealing with pediatric cancer recurrence?
Parents dealing with pediatric cancer recurrence can access various resources, including support groups, counseling services, and educational materials from cancer organizations. Institutions may also provide specialized programs to help families navigate treatment options and long-term care strategies.
| Key Point | Details |
|---|---|
| AI Tool Efficiency | An AI tool predicted pediatric cancer recurrence with higher accuracy than traditional methods (75-89% vs 50%). |
| Research Collaboration | Conducted by Mass General Brigham, Boston Children’s Hospital, and Dana-Farber, leveraging 4,000 MR scans from 715 patients. |
| Temporal Learning | A unique method where AI analyzes multiple scans over time to identify subtle changes indicating recurrence. |
| Clinical Applications | Aims to improve patient care by identifying high-risk patients and potentially reducing unnecessary imaging. |
| Future Directions | Further validation needed with plans for clinical trials to enhance treatment based on AI predictions. |
Summary
Pediatric cancer recurrence remains a significant concern for healthcare providers and families alike. The recent study highlighting the use of an AI tool demonstrates a promising advancement in predicting relapse risks among pediatric patients suffering from gliomas. By employing temporal learning techniques, researchers have improved the accuracy of these predictions, potentially allowing for more tailored treatment strategies and better outcomes. This innovation could reshape how practitioners monitor childhood cancer, emphasizing the need for continued exploration and application of AI in the medical field.