Recent studies are shining a light on the potential role of TIM-3 in the fight against Alzheimer’s disease, raising hopes for innovative Alzheimer’s treatment options. TIM-3, a checkpoint molecule typically associated with immune regulation, has been found to impact the functioning of microglia—brain cells responsible for clearing amyloid plaques linked to cognitive decline. By understanding how TIM-3 therapy can enhance microglial activity, researchers are exploring new avenues for cognitive function improvement in patients suffering from this debilitating condition. As the medical community delves deeper into the interactions between the immune system and Alzheimer’s, the findings suggest that targeting TIM-3 could be a game-changer in combating memory loss and enhancing the quality of life for those affected by Alzheimer’s. Overall, the linkage between TIM-3 and the immune response could lead to groundbreaking advancements in Alzheimer’s disease management.
The exploration of TIM-3’s involvement in Alzheimer’s disease opens a new chapter in understanding the immune response mechanisms underlying neurodegeneration. This checkpoint protein is drawing attention not only for its role in regulating the brain’s immune cells but also for its potential implications in developing effective Alzheimer’s treatment strategies. Researchers are now focusing on how TIM-3 influences microglia’s ability to manage amyloid plaque accumulation, a key factor in cognitive decline. By enhancing this immune response, scientists aim to stimulate cognitive function improvement and better manage Alzheimer’s symptoms. The intriguing relationship between the immune system and this neurodegenerative disease highlights the need for innovative therapeutic approaches and further studies into TIM-3’s multifaceted role.
The Role of TIM-3 in Alzheimer’s Disease
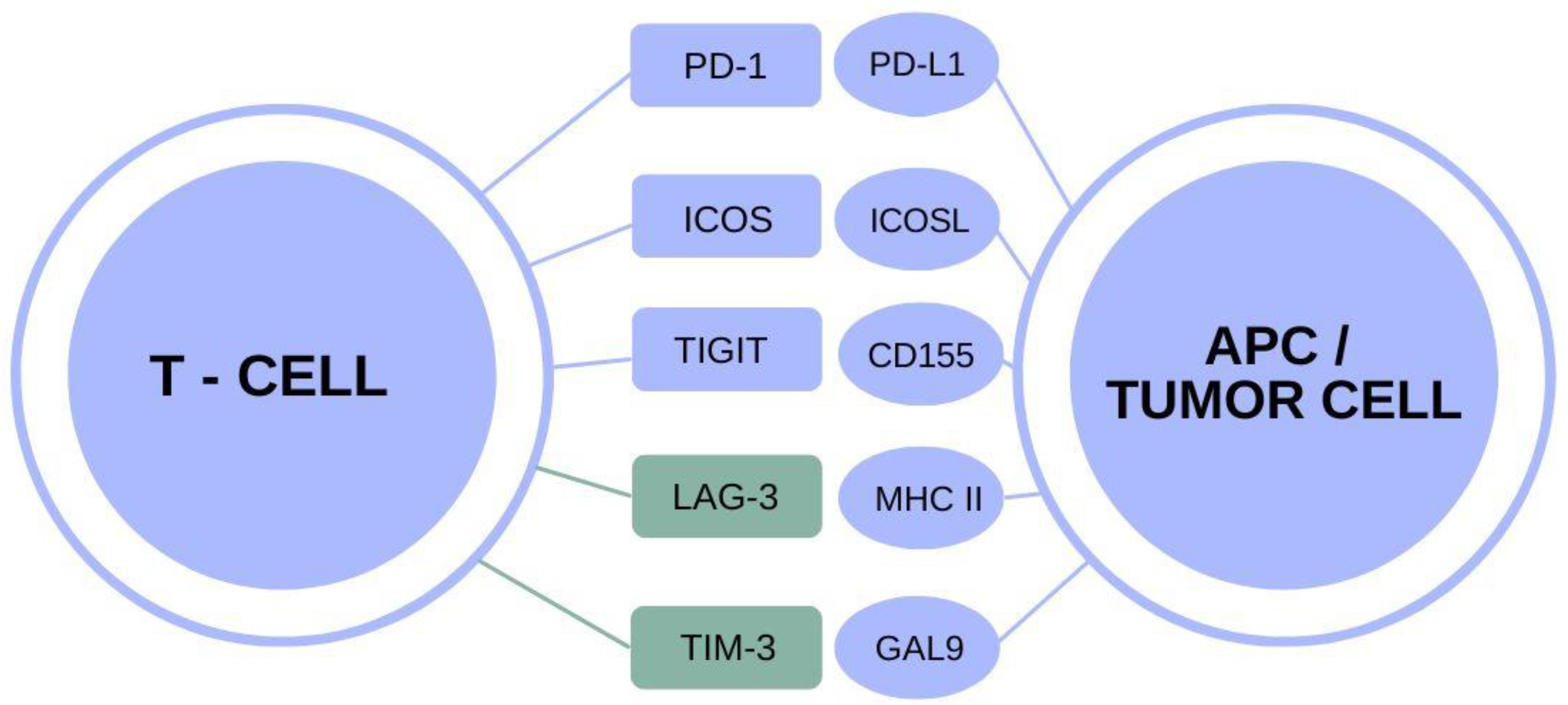
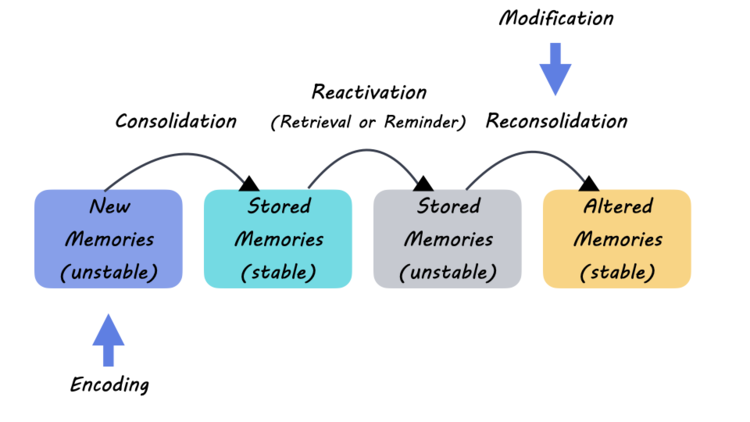
TIM-3, or T cell immunoglobulin and mucin domain 3, has emerged as a significant player in the pathology of Alzheimer’s disease (AD). This immune checkpoint molecule is heavily expressed on microglia, the brain’s resident immune cells, particularly in the context of AD where amyloid-beta plaques accumulate. Its upregulation indicates a crucial mechanism by which microglia are impeded from performing their primary role—clearing these harmful plaques. In studies, it has been observed that deleting the TIM-3 gene leads to enhanced microglial activity, enabling these cells to effectively reduce plaque burden, subsequently improving cognitive functions in experimental models. This suggests that TIM-3 acts not merely as a passive marker but as an active regulator of microglial response in the Alzheimer’s landscape.
Moreover, the connection of TIM-3 to late-onset Alzheimer’s disease establishes it as a potential genetic risk factor for the illness. Research indicates that certain polymorphisms of the TIM-3 gene correlate with an increased risk of developing AD. As such, TIM-3 is positioned at the intersection of immune response and neurodegeneration, influencing how effectively the brain can respond to plaque accumulation common in Alzheimer’s. Identifying and targeting TIM-3 could not only elucidate the mechanisms behind cognitive decline in AD patients but also pave the way for novel therapeutic strategies.
Frequently Asked Questions
What is the role of TIM-3 in Alzheimer’s disease and how does it relate to immune system functions?
TIM-3, an immune checkpoint molecule, is significant in Alzheimer’s disease (AD) as it inhibits microglia, the brain’s immune cells, from clearing amyloid plaques. In Alzheimer’s patients, TIM-3 is expressed at higher levels, preventing microglia from attacking these harmful plaques, which leads to cognitive decline.
How can TIM-3 therapy potentially improve Alzheimer’s treatment outcomes?
TIM-3 therapy could enhance Alzheimer’s treatment by blocking the inhibitory function of TIM-3, thereby enabling microglia to effectively clear amyloid plaques from the brain. This may restore cognitive functions that are impaired in Alzheimer’s patients.
What are the implications of microglia expressing TIM-3 in the context of Alzheimer’s disease?
The expression of TIM-3 by microglia in Alzheimer’s disease results in their inability to clear amyloid plaques, contributing to the progression of cognitive decline. By targeting TIM-3, researchers aim to reactivate the plaque-clearing abilities of microglia, improving cognitive function.
Can TIM-3 anti-body therapy be safely used in treating Alzheimer’s disease?
Yes, TIM-3 antibody therapy shows promise for safely treating Alzheimer’s disease. Existing anti-TIM-3 antibodies may be repurposed to enhance microglia function specifically, minimizing vascular risks associated with traditional anti-amyloid therapies.
How does TIM-3 impact memory restoration in Alzheimer’s mouse models?
In Alzheimer’s mouse models, deleting TIM-3 allows microglia to clear amyloid plaques, which has been shown to improve cognitive function and memory. This suggests that targeting TIM-3 could lead to significant advancements in Alzheimer’s treatment.
What is the current state of research on TIM-3 and Alzheimer’s disease therapy?
Current research is focused on investigating the efficacy of human anti-TIM-3 antibodies in halting plaque development in Alzheimer’s disease mouse models. This could pave the way for developing novel therapeutic approaches for humans with Alzheimer’s.
How does TIM-3 compare to other therapies available for Alzheimer’s treatment?
TIM-3 therapy represents a novel approach compared to existing Alzheimer’s treatments, targeting the immune response and enhancing the brain’s natural ability to clear amyloid plaques, rather than solely focusing on amyloid beta levels.
What are the potential benefits of blocking TIM-3 in Alzheimer’s patients?
Blocking TIM-3 may reactivate microglia, allowing them to diminish amyloid plaque accumulation, potentially leading to improved cognitive functions, reduced Alzheimer’s symptoms, and enhanced overall brain health.
What challenges do scientists face in translating TIM-3 research into human therapies?
Challenges include ensuring the safety and efficacy of TIM-3 therapies in humans, understanding the complex role of immune mechanisms in Alzheimer’s, and navigating the regulatory landscape for new treatment modalities.
What is the significance of the relationship between TIM-3 and cognitive function improvement in Alzheimer’s disease?
The relationship between TIM-3 and cognitive function improvement in Alzheimer’s disease highlights the potential for innovative therapies targeting immune mechanisms to restore cognitive processes, making it a critical area of ongoing research.
| Key Points | Details |
|---|---|
| Research Topic | The use of TIM-3 regulation in Alzheimer’s disease. |
| Key Finding | Deleting TIM-3 in mice led to plaque clearance and improved cognition. |
| Molecule of Interest | TIM-3 is a checkpoint molecule that inhibits microglial activity. |
| Link to Alzheimer’s Disease | TIM-3 expression is linked to the genetic risk factor for late-onset Alzheimer’s. |
| Clinical Implications | Potential for repurposing anti-TIM-3 antibodies in Alzheimer’s treatment. |
| Model Used in Research | Transgenic mice with the TIM-3 gene deleted were used for experiments. |
| Research Duration | The study took five years to complete, with many experiments conducted. |
Summary
TIM-3 and Alzheimer’s Disease represent a promising frontier in neurological research, revealing that targeting the TIM-3 checkpoint molecule may enhance microglial functionality and cognitive preservation. This innovative strategy suggests that repurposing cancer therapies could lead to transformative treatments in Alzheimer’s, potentially improving outcomes for those affected by this debilitating disease.