Maternal mortality remains a critical concern in the United States, where pregnancy-related deaths continue to rise alarmingly. Despite advancements in healthcare, this high-income nation has the highest maternal mortality rate among its peers, with over 80 percent of these tragic outcomes deemed preventable. Recent studies have highlighted severe disparities in maternal health care, revealing significant racial inequalities that contribute to the overall mortality rate. Issues such as inadequate postpartum care and systemic biases only exacerbate the problem, putting vulnerable populations at greater risk. Addressing these issues is vital, as ensuring equitable access to quality maternal health care can prevent many of these unnecessary deaths.
The discussion around maternal mortality is underscored by the broader issue of pregnancy-related fatalities, which highlight the urgent need for systemic improvements. Many of these fatalities are preventable, yet the rates are on an unsettling upward trend, signaling an urgent call for reform in maternal health systems. Particularly alarming are the disparities in outcomes among different racial groups, which point to systemic inequalities that must be addressed. Furthermore, the importance of comprehensive postpartum support cannot be overstated, as inadequate care during this period significantly contributes to maternal deaths. As we explore these interconnected factors, it becomes clear that a multifaceted approach is necessary to combat the growing crisis of maternal mortality.
Rising Trends in Maternal Mortality Rates in the U.S.
Recent studies indicate alarmingly increasing trends in maternal mortality in the United States. Between 2018 and 2022, the nation recorded a troubling increase in pregnancy-related deaths, culminating in a rate of 32.6 deaths per 100,000 live births by 2022, compared to 25.3 in 2018. The sharpest increase was seen in 2021, potentially exacerbated by the health impacts of the COVID-19 pandemic, which disrupted healthcare access and prenatal care for many expectant mothers. Furthermore, these figures reveal significant geographic and racial disparities, making it crucial to focus on systemic factors that contribute to such preventable deaths in our society.
The higher mortality rates in the U.S. compared to other high-income countries highlight critical issues within the American healthcare system, including inconsistent maternal health care access and inadequate postpartum support. Addressing these rising trends necessitates a multi-faceted approach that targets the underlying causes of maternal mortality. This includes investing in comprehensive prenatal care, ensuring equitable access to quality pregnant care services, and focusing on reducing disparities faced by marginalized groups to ultimately decrease the alarming statistics surrounding maternal health.
Preventable Deaths and the Importance of Quality Maternal Health Care
With over 80% of pregnancy-related deaths identified as preventable, there is an urgent need to improve maternal health care systems across the United States. Ensuring that women receive timely and adequate prenatal care, continuous support during pregnancy, and effective postpartum care can drastically reduce these fatalities. Public health initiatives should prioritize equitable access to these essential services, addressing the barriers that disproportionately affect underrepresented groups, including American Indian, Alaska Native, and Black women, who experience the highest maternal mortality rates.
Furthermore, implementing standardized protocols across healthcare facilities can enhance the quality of maternal health care. This includes training medical practitioners to recognize and manage high-risk pregnancies more effectively and providing education on signs of postpartum complications. By focusing on innovative solutions designed to improve care throughout the entire maternity continuum, we can ultimately reduce the number of preventable deaths associated with pregnancy and childbirth.
The Role of Postpartum Care in Maternal Health Outcomes
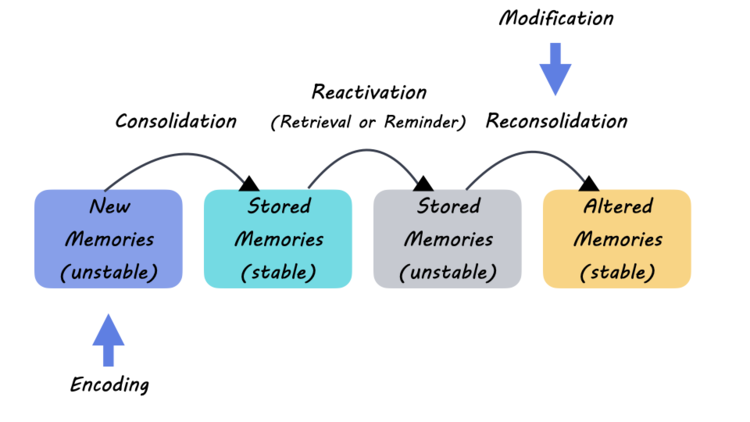
Postpartum care is a critical aspect of maternal health often overlooked, yet it is essential in mitigating maternal mortality. The World Health Organization currently recognizes maternal deaths occurring within 42 days postpartum, but recent studies suggest that the crucial recovery period can extend well beyond this arbitrary timeframe. In fact, nearly a third of maternal deaths in recent years occurred during the late postpartum phase, highlighting the need to broaden care practices and support for new mothers well into their first year after childbirth.
Improving extended postpartum care can significantly impact health outcomes, ensuring women receive ongoing support and monitoring for issues like hypertension and mental health challenges. Health systems must adapt to treat postpartum recovery as a continuous journey rather than a short-term phase, providing education, follow-up care, and interventions tailored to each woman’s needs. Doing so could play a pivotal role in preventing many mortality cases that currently go unaddressed.
Addressing Racial Disparities in Maternal Mortality
One of the most alarming insights from recent studies is the stark racial disparities in maternal mortality rates. Data reveals that American Indian and Alaska Native women face mortality rates nearly four times higher than their white counterparts. This statistic highlights systemic issues within the healthcare system, including access to quality care and the potential presence of bias in medical treatment decisions. Addressing these inequitable practices is crucial for the health of all mothers.
Innovative solutions are necessary to specifically target and ameliorate the factors contributing to these racial disparities. Increasing diversity in healthcare providers, ensuring cultural competence in care, and implementing community-driven maternal health programs can help bridge the gap. By actively involving affected communities in health initiatives and policy-making, we can foster environments that support informed pregnancy and birth experiences, ultimately reducing maternal mortality across diverse populations.
Investment in Public Health Infrastructure for Maternal Health
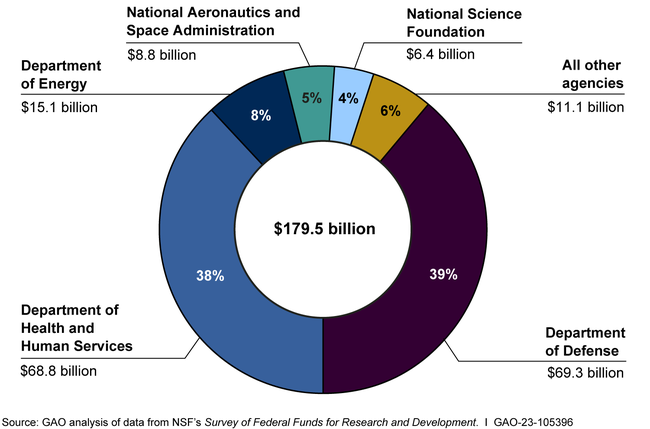
Investing in public health infrastructure is paramount for improving maternal health outcomes in the U.S. Current trends show that without decisive action, rates of pregnancy-related deaths are not only stagnant but worsening. This calls for a systematic allocation of resources towards better tracking of maternal health indicators, workforce training, and the establishment of comprehensive care models that prioritize women’s health before, during, and after childbirth.
Moreover, state and federal governments must confer importance on maternal health by allocating sufficient funding for research and evidence-based programs. By enhancing data collection systems and improving access to quality maternal health care across all regions, we can reduce the disproportionate impact of maternal deaths and enhance pregnancy experiences nationwide. Continued support for public health initiatives is not merely an investment in mothers but is foundational for the health of families and communities as a whole.
Understanding the Impact of Chronic Conditions on Maternal Mortality
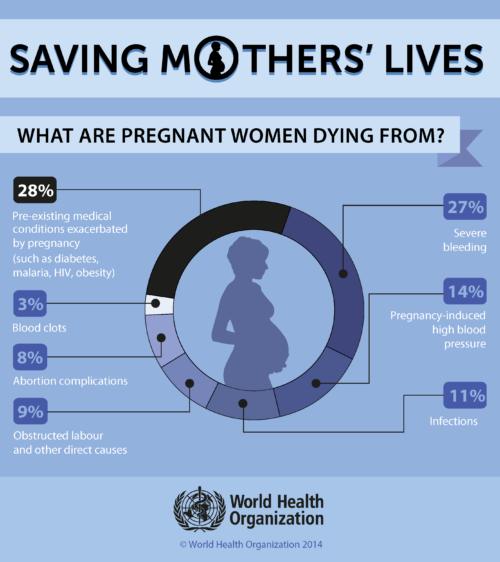
Chronic conditions like hypertension, diabetes, and cardiovascular disease have a significant impact on maternal mortality rates. Recent studies indicate that an increasing number of reproductive-aged individuals are developing severe chronic health conditions, leading to higher risks during pregnancy. With cardiovascular disease emerging as the leading cause of pregnancy-related death in the U.S., healthcare providers must be vigilant in managing these underlying conditions to mitigate risks associated with pregnancy.
This emphasis on understanding and treating chronic illnesses in pregnant women opens the door to innovative screening and management strategies. Early intervention protocols and personalized care plans can be instituted to monitor and support women with chronic conditions throughout their pregnancies. Adequate medical supervision, tailored education, and coordinated care across healthcare specialties can ultimately lead to improved maternal health outcomes, substantially decreasing preventable deaths.
Strategies to Improve Prenatal Care Access and Quality
Ensuring that all pregnant individuals have access to high-quality prenatal care is integral to reducing preventable maternal deaths. This involves addressing systemic barriers, such as economic disparities and geographic limitations, that hinder access to healthcare services. By implementing policies that provide financial assistance for low-income mothers and expanding healthcare facilities in underserved areas, we can significantly improve the pregnancy experience and health outcomes for vulnerable populations.
Moreover, quality improvement initiatives in hospitals and clinics are essential for enhancing prenatal care. Training healthcare providers in recognizing early warning signs and promoting best practices for maternal care can directly influence treatment outcomes. Furthermore, community outreach programs offering education about maternal health and prenatal resources can empower mothers to engage with the healthcare system effectively, ultimately leading to better health for both mothers and their newborns.
The Importance of Data Tracking in Maternal Health
Accurate data tracking is essential for understanding the scope of maternal mortality in the U.S. The implementation of pregnancy checkboxes on death certificates has contributed significantly to collecting better data on pregnancy-related deaths since 2018. Despite these advancements, continuous efforts are needed to ensure comprehensive tracking and reporting of maternal deaths, which center around identifying trends and risk factors that could help develop targeted interventions.
Moreover, involving interdisciplinary approaches in data collection can help capture a broader understanding of factors influencing maternal health. Leveraging big data analytics and community health assessments can reveal systemic issues that contribute to maternal deaths, aiding policymakers in crafting actionable solutions. Ultimately, reliable data will inform public health strategy, fostering initiatives aimed at reducing maternal mortality rates across diverse demographics.
Legal and Policy Reforms for Improved Maternal Health Outcomes
To address the rising rates of maternal mortality and the systemic barriers faced by women of color, comprehensive legal and policy reforms are vital. Legislative measures that prioritize maternal health funding, protect women’s healthcare rights, and promote access to affordable and quality care should be at the forefront of public health initiatives. These reforms can create a more supportive environment for expecting mothers and incentivize healthcare providers to prioritize maternal health.
Additionally, advocating for policies that directly address social determinants of health can lead to better outcomes for mothers and their children. This involves recognizing how factors like housing, education, and income directly impact maternal health. Comprehensive policies that aim to improve overall community welfare can contribute to more sustainable and equitable health outcomes, thereby reducing rates of maternal mortality.
Frequently Asked Questions
What are the main factors contributing to high maternal mortality in the U.S.?
The high rate of maternal mortality in the U.S. can be attributed to several factors including a fragmented healthcare system, inequitable policies, the presence of maternity care deserts, and systemic bias against racial and ethnic groups. Moreover, the increasing prevalence of chronic medical conditions, such as hypertension and cardiovascular diseases among younger individuals, contributes to this alarming trend.
How do racial disparities impact maternal mortality rates in the U.S.?
Racial disparities significantly affect maternal mortality rates, with American Indian and Alaska Native women experiencing the highest rates of pregnancy-related deaths. Research indicates that these inequities persist due to social determinants of health and systemic inequities in maternal health care access, highlighting the need for targeted interventions to improve outcomes for all racial groups.
Why is postpartum care crucial in reducing maternal mortality?
Postpartum care is essential in the fight against maternal mortality as nearly a third of maternal deaths occur between six weeks and one year after pregnancy. Improving postpartum healthcare systems to address the continuum of care beyond the initial weeks can help in recognizing and managing postpartum complications, thus potentially reducing preventable deaths.
What types of deaths are classified as pregnancy-related, and how do we track them?
Pregnancy-related deaths include those occurring during pregnancy and shortly after childbirth. Since 2018, a national system has been implemented to track these deaths, thanks to a pregnancy checkbox on death certificates. However, there’s a push to expand this definition to include late maternal deaths, which highlights the significance of prolonged postpartum care.
What steps can be taken to lower U.S. maternal mortality rates?
To lower maternal mortality rates in the U.S., it is crucial to invest in public health infrastructure, enhance maternal health care services, and address disparities at the state level. Implementing comprehensive policies that promote better healthcare access and quality of care during pregnancy and the postpartum period can effectively reduce preventable deaths.
How has the COVID-19 pandemic affected maternal mortality rates?
The COVID-19 pandemic has had a detrimental effect on maternal mortality rates, particularly in 2021, which saw the sharpest increase in deaths. The pandemic exacerbated existing disparities in health care access and likely contributed to worsening maternal health outcomes due to the strain on healthcare systems and resources.
What trends have been observed in maternal health care over the years?
Over the years, there’s been a significant shift in the leading causes of pregnancy-related deaths from hemorrhage to cardiovascular disease. This shift indicates a growing concern about chronic health issues such as hypertension, especially among younger women, which has become a major factor in maternal mortality.
What role do public health investments play in improving maternal health outcomes?
Public health investments are crucial for improving maternal health outcomes. Increased funding and focus on innovative solutions in maternal health care can enhance the quality of care during pregnancy and postpartum, ultimately lowering rates of preventable deaths and addressing systemic disparities.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality Rate | The U.S. continues to have the highest maternal mortality rate among high-income countries, which has risen from 25.3 in 2018 to 32.6 deaths per 100,000 live births in 2022. |
| Preventability of Deaths | More than 80% of the pregnancy-related deaths are preventable with better healthcare. |
| Disparities in Death Rates | Significant racial disparities exist, with American Indian and Alaska Native women facing the highest rates (106.3 per 100,000), followed by non-Hispanic Black women (76.9) and white women (27.6). |
| Impact of COVID-19 | The sharpest increase in mortality rates occurred in 2021, likely due to the COVID-19 pandemic. |
| Chronic Conditions | Cardiovascular disease is now the leading cause of pregnancy-related death, reflecting a trend of increasing chronic conditions in younger populations. |
| Need for Better Care Postpartum | Late maternal deaths (occurring after 42 days postpartum) account for nearly a third of total maternal deaths, suggesting a need for care extending beyond traditional timeframes. |
| Public Health Infrastructure | Investment in public health infrastructure is critical, as current rates indicate a worsening situation rather than improvement. |
Summary
Maternal mortality remains a pressing issue in the U.S., with rising rates posing a significant public health concern. As highlighted by recent research, the predominantly preventable nature of these deaths underscores the urgent need for enhanced prenatal and extended postpartum care. With disparities across race and state, targeted interventions and investments in healthcare infrastructure are essential to drive down maternal mortality and safeguard the health of mothers and newborns alike.